Dialectical Behavior Therapy (DBT): What It Is and How It’s Used

If you’ve been struggling with intense emotions and looking into professional support, you might have come across Dialectical Behavior Therapy, also known as DBT.
DBT is a form of talking therapy which has been adapted from Cognitive Behavioral Therapy (CBT) for people who struggle with managing their intense emotions. It’s often recommended for people with severe mood disorders, but it can be used to treat a wide range of mental health conditions – and its core elements can be used to help anyone to build emotional regulation skills.
Today, we’ll dive into the history and theory behind DBT, what DBT is used for, DBT vs. CBT, what happens in DBT, and how DBT might help with attachment difficulties. Keep reading to find out everything you need to know about DBT…
Disclaimer: This article includes discussion of suicide and self-harm. If you’re affected by the contents of this article, please seek support from a mental health professional.
DISCOVER YOUR ATTACHMENT STYLE
What Is DBT Therapy?
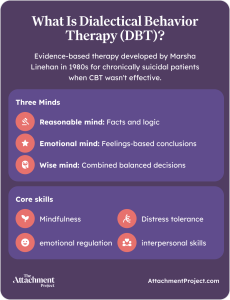
Dialectical Behavior Therapy is an evidence-based psychotherapy which was developed in the 1980s by psychologist Marsha M. Linehan. It grew out of a need to better treat chronically suicidal patients, specifically women, as CBT protocols of the time were not effective1. It was first used as a treatment for borderline personality disorder (BPD), and remains the top psychotherapy for BPD, though it can now be applied to a wide range of mental health conditions involving emotional dysregulation.
“Dialectical” describes the idea of holding two opposite ideas at the same time. In DBT, one way this is conceptualized is that we have both a “reasonable mind”, based in facts and logic, and an “emotional mind”, which draws conclusions based on feelings2. The reasonable mind and emotional mind can contradict each other, but both can have a point; combining them results in the “wise mind”, a place from which we can make decisions that are grounded in logic but still informed by our feelings.
Mindfulness, distress tolerance, emotional regulation, and interpersonal (relationship) skills are central to DBT1. Combining these skills can help us to accept ourselves and others in more balanced ways, leading to better mental health and more stable relationships. We’ll go over some examples of how DBT can be applied soon.
What Is DBT Therapy Used For?
So, is DBT only for personality disorders? Although DBT was originally conceived to assist in the treatment of borderline personality disorder, mental health professionals now recognize how valuable its core skills can be in anyone struggling with emotional dysregulation and impulsivity. Evidence has been found for its effectiveness in treating a wide range of mental health conditions, including1:
- Self-harm
- Suicidal ideation and/or attempts
- Mood disorders such as depression
- Eating disorders or disordered eating
- Post Traumatic Stress Disorder (PTSD)
- Addiction, such as drug and alcohol dependence
Although DBT is widely applicable to a range of conditions, it isn’t necessarily the right therapy for everyone. To get the best out of DBT, you need to be prepared to engage in group skills-building sessions, focus on your present and future circumstances instead of the past, and complete work between sessions.
DBT vs. CBT: Key Differences Explained
To help clearly define the differences between Dialectical Behavior Therapy and Cognitive Behavioral Therapy, we break these down into philosophical differences and treatment differences:
Philosophical Differences
| CBT | DBT |
|---|---|
| CBT focuses on reasoning, rationale, and critical thinking to challenge assumptions and beliefs. | DBT focuses on mindfulness techniques to help people accept the things they cannot change in life, instead of struggling to try to change them, including emotional pain. |
Treatment Differences
| CBT | DBT |
|---|---|
| CBT targets the cycle of thoughts, feelings, behaviors, and actions. It teaches people the skills to recognize problematic thoughts and techniques for redirecting them. | DBT also focuses on thoughts, feelings, behaviors, and actions, but more on how to accept and regulate these factors through mindfulness and managing destructive behaviors as a result. |
DBT Therapy Techniques
The main aim of DBT therapy is to forge a balance between developing acceptance of you as an individual, along with the challenges and flux of change.
Although the nuances of DBT can vary from therapist to therapist, DBT treatment techniques typically follow a set structure.
The Stages of DBT Therapy Explained
In general, DBT involves four types of sessions:
- Pre-assessment
- Individual therapy
- Group therapy skills training
- Over-the-phone crisis coaching
DBT Pre-Assessment
A therapist will usually determine whether DBT is suitable for your needs through a pre-assessment meeting. During pre-assessment, they will likely ask a few questions about your symptoms and experiences, as well as describe how DBT works. If you decide that DBT is the right therapeutic route for you, they’ll ask whether you’re ready to commit to the duration of therapy.
Individual Therapy
Individual therapy in DBT involves weekly one-to-one sessions with your therapist which usually last a set time of between 40-60 minutes.
During therapy sessions, a DBT therapist aims to help you to set and reach treatment goals by targeting blockages to progress, such as current mental well-being issues or relational difficulties, recognize and reduce harmful thoughts and behaviors, target maladaptive behavioral patterns, and replace harmful behaviors with new, helpful skills.
Group Therapy Skills Training
Skills training often happens in groups, but don’t worry – this doesn’t mean you’ll have to talk about personal and difficult topics in a group setting. Skills-based therapy groups aim to teach new techniques for managing thoughts and emotions, focused on the here and now instead of the past.
Group skills training sessions teach people techniques such as mindfulness, distress tolerance, boundary setting and expression of needs, as well as emotion regulation practices.

Over-the-Phone Crisis Coaching
People in DBT are already likely to experience emotional crises. DBT therapists recognize that these can happen at any time, including outside of therapy sessions. DBT is different to most therapeutic approaches in that therapists are available for crisis coaching at any time – while it’s not realistic to expect anyone to be constantly contactable, DBT therapists will provide guidance and model boundary setting around when and why you can call them for support outside of sessions.
Who Can Benefit from DBT Therapy?
Anyone struggling to manage their intense emotions and the distress these emotions cause – as well as any resulting harmful behaviors – could benefit from DBT. These emotions could be caused by mental health conditions such as borderline personality disorder, mood disorders such as anxiety and depression, PTSD, or any mental health condition which affects your well-being.
Dialectical Behavior Therapy may also be suitable for people who have tried other kinds of therapy in the past and felt they didn’t benefit from it. Since it focuses on acceptance, the present, and the future more than many other forms of therapy, it can be particularly helpful if therapy based on exploring the past isn’t helpful for you.
DBT for ADHD: How It Works
A developmental disorder previously treated mainly with medication, attention deficit hyperactivity disorder (ADHD) is now sometimes treated with a combination of medication and DBT. DBT’s effectiveness for treating ADHD is associated with its ability to target the feelings of overwhelm and intense emotions associated with ADHD, while medication may help to manage its cognitive aspects like organization and time management3.
Implementing behavior change can be difficult for people with ADHD, but DBT focuses on self-regulation skills for improving emotion management and developing the “wise mind”. A DBT therapist’s role is to help someone with ADHD to recognize what they can change and what they can accept in their life, identify behavioral and thinking patterns, and learn strategies for dealing with impulsivity.
DBT Therapy for Depression
DBT teaches people skills for regulating emotions and coping with the challenges of day-to-day life. Depression is a condition characterized by feelings of persistent low mood and difficulties coping with activities and tasks associated with everyday life. Therefore, DBT can be very helpful in the treatment of depression, as it teaches people how to manage a major depressive episode and the negative emotions associated with it4.
In many cases, medication may be necessary in conjunction with DBT to effectively treat depression. It’s recommended to speak to a local medical health professional for guidance if you’re concerned about your mental health.
Treating OCD with DBT Techniques
Obsessive compulsive disorder (OCD) is a mental health condition characterized by intrusive thoughts and repetitive behaviors (known as obsessions and compulsions). DBT helps people with OCD to manage their feelings of anxiety and distress by focusing on acceptance, non-judgment, and mindfulness5.
In this way, clients can begin to free themselves from obsessions and compulsions by learning how to live in the moment, understand the source of their difficulties, and distract themselves from distressing feelings.
DBT Therapy for PTSD
Post traumatic stress disorder (PTSD) is a condition in which people find it difficult to readjust to normal life after a traumatic event. They may re-experience aspects of the trauma, exhibit trauma responses in day to day life, and find it difficult to relate to other people. They also have a lower “window of tolerance” – the amount of any kind of stress they can tolerate – making them prone to emotional dysregulation.
DBT emphasizes that distress and emotional pain are often a part of life, but that we can live a functional life regardless. Through implementing techniques such as mindfulness, acceptance, validation, and perspective-taking, DBT can help people suffering with PTSD to cope with their distressing emotions and challenges relating to others6. With time, they can practice skills for optimal recovery at home, in relationships, and at work.
Managing Anxiety with DBT Skills
Cognitive behavioral therapy (CBT) is often the go-to therapy for treating anxiety. However, DBT can be highly effective for treating the intense emotions that often accompany anxiety disorders, especially the socio-emotional aspects of anxiety. Through skills such as mindfulness, distress tolerance, and interpersonal effectiveness, DBT helps people to cope with the stressors of their environment in less emotional and more productive ways7.
Real Examples of DBT Therapy
The following are some examples of DBT skills which can be applied to everyday life scenarios.
The “STOP Skill”
STOP is an acronym for Stop, Take a step back, Observe, and Proceed mindfully. It is a particularly effective technique for when emotions feel overwhelming or out of control. The STOP Skill can be used in everyday scenarios such as the following:
Say you’re feeling angry about a conflict you had with your boss at work. Your impulse is to go into their office and tell them exactly what you think. Stop for a moment, Take a step back from your distressing thoughts, and Observe your thoughts without judgment. Then, when you have achieved some clarity on the situation, Proceed. You might decide that the best course of action is to seek advice from a co-worker, look for support from a loved one, or tackle the conflict in a non-confrontational manner. Regardless, the STOP Skill gives you the ability to pause and gain insight into a situation before you react, effectively breaking the cycle of distress and anxiety and creating the space for you to proceed from a more rational perspective.

The “Opposite Action” Technique
The Opposite Action technique involves literally doing the opposite of what your emotions are telling you to do. The theory behind this technique is that doing the opposite action is the most effective way to calm the emotion, while at the same time curbing your impulses.
For example, say you’re feeling down and your impulse is to stay in bed all day. The Opposite Action would be to get up and do something high-energy and active, like dance or go for a run. When you’re done, it’s likely that you won’t feel as low as you did before, and you might be able to carry out your daily activities.
DBT Therapy and Attachment
If you have an insecure attachment style, you might find it more difficult to cope with your emotions. Research has found that people high in attachment avoidance are less able to recognize their emotions, so may underreact to them, while people high in attachment anxiety can feel emotions more intensely (though they may still find it difficult to identify them) and struggle with impulsivity8.
By now, you know that DBT can be particularly useful for emotional regulation and relating to others. If attachment difficulties form part of your mental health challenges, DBT could help you to manage these and build more secure relationships with others.
Conclusion
Even though dialectical behavior therapy was originally devised to help suicidal patients who weren’t benefitting from other kinds of therapy, its teachings on emotional regulation and interpersonal skills can be applied to almost any mental health difficulty involving these challenges.
If you think DBT could be right for you, get in touch with a DBT therapist or your existing mental health provider. If you’re interested in learning more about your attachment style and how it could be contributing to emotional dysregulation, start by taking our free attachment quiz.
References
- Robins, C. J., & Chapman, A. L. (2004). Dialectical behavior therapy: Current status, recent developments, and future directions. Journal of Personality Disorders, 18(1), 73–89.
- Linehan, M. M. (2015). DBT skills training manual (2nd ed.). The Guilford Press.
- Basiri N. The Effects of Dialectical Behavioural Therapy (DBT) on Cognitive and Emotional Symptoms of Adult ADHD: A Randomised Pilot Study. Counselling and Psychotherapy Research. 2025 Mar;25(1):e12900.
- Khani H, Belir S, Zamani S, Zamani N. Efficacy of dialectical behavior therapy on depression. Journal of Mazandaran University of Medical Sciences. 2015 Aug 10;25(127):113-8.
- Ahovan M, Balali S, Shargh NA, Doostian Y. Efficacy of dialectical behavior therapy on clinical signs and emotion regulation in patients with obsessive-compulsive disorder. Mediterranean Journal of Social Sciences. 2016 Jul;7(4):412.
- Oppenauer, C., Sprung, M., Gradl, S., & Burghardt, J. (2023). Dialectical behaviour therapy for posttraumatic stress disorder (DBT-PTSD): Transportability to everyday clinical care in a residential mental health centre. European Journal of Psychotraumatology, 14(1), 2157159.
- Malivoire BL. Exploring DBT skills training as a treatment avenue for generalized anxiety disorder. Clinical Psychology: Science and Practice. 2020 Dec;27(4):20.
- Stevens FL. Affect regulation styles in avoidant and anxious attachment. Individual Differences Research. 2014 Sep 1;12(3).








 Get mental health tips straight to your inbox
Get mental health tips straight to your inbox